Atrial fibrillation is one of the most common heart rhythm problems seen worldwide today. With ongoing research and advances in heart care, new recommendations and updated guidelines have been released to help doctors and patients better prevent complications, improve quality of life, and tailor treatments. In this blog, we will explain what has changed in the 2026 update for managing atrial fibrillation, and why these changes matter in simple Indian English. Along the way, we will also explain how to find the best cardiology doctor for you or your loved one.
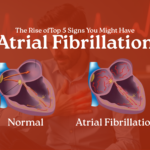
What is Atrial Fibrillation?
Atrial fibrillation (often called AF or AFib) happens when the top chambers of the heart — the atria — start beating in an irregular and often fast rhythm. This irregular heartbeat can lead to poor blood flow, dizziness, chest discomfort, shortness of breath, and, importantly, an increased risk of stroke and heart failure. The risk of atrial fibrillation increases with age and in people with other conditions such as high blood pressure, diabetes, or heart disease.
Why Do Guidelines Change?
Guidelines for managing atrial fibrillation are updated regularly because new research helps doctors understand better ways to prevent complications, treat symptoms, and improve long-term outcomes. The latest update in 2026 focuses on a more holistic and patient-centred approach to atrial fibrillation care. The updates are based on evidence from new international studies and expert consensus.
Key Changes in the 2026 Atrial Fibrillation Guidelines
Here are the important changes that doctors and patients should know about:
1. More Focus on Patient-Centred, Integrated Care
Historically, treatment focused mostly on controlling heart rate and preventing strokes. The latest guidelines emphasise a patient-centred care approach that includes lifestyle, comorbid conditions, and overall heart health. This means treatment is no longer only about medications, but also about understanding each patient’s risks, preferences, and lifestyle.
Doctors are advised to work in a multi-disciplinary team that includes general physicians, cardiologists, nurses, and other specialists to deliver coordinated care. Shared decision-making between doctor and patient is strongly encouraged.
2. Better Use of Rhythm-Control Strategies
Earlier guidelines focused first on slowing the heart rate and only later considering rhythm control (bringing the heart back to a normal rhythm). Now there is a greater emphasis on early rhythm control, especially in patients who are newly diagnosed or at high risk. This can include medications, electrical cardioversion, or catheter ablation procedures that target the source of irregular signals in the heart. Early rhythm control has been shown to reduce symptoms, lower risk of hospitalisation, and possibly improve long-term outcomes in some patients.
3. Stroke Prevention and Anticoagulation Guidance Updated
Stroke prevention remains a core part of managing atrial fibrillation. New evidence has helped doctors better balance bleeding risk with stroke prevention.
Doctors now use updated risk scores to decide who needs blood thinners like anticoagulants. These medications help prevent clots that can cause strokes. The guidelines also cover how to manage people with device-detected atrial fibrillation (e.g., detected by smart wearables), and when long-term anticoagulation is recommended.
4. Comprehensive Comorbidity Management
The updated guidelines put significant weight on managing other health problems that often occur with atrial fibrillation — such as high blood pressure, diabetes, sleep apnea, and heart failure. Treating these conditions well can reduce the burden of atrial fibrillation and improve outcomes.
This approach is part of a care pathway sometimes called “AF-CARE” (Comorbidity management, Avoidance of stroke, Rate/rhythm control, and Evaluation and dynamic reassessment).
5. Technology and Risk Assessment Tools
The 2026 update also acknowledges the growing role of technology in detecting and monitoring atrial fibrillation. Wearables and AI-aided tools are now being better studied so that atrial fibrillation can be detected earlier, and doctors can personalise treatment based on risk.
While these tools are not meant to replace a medical diagnosis or expert review, they help both patients and doctors make more informed decisions.
Tips to Manage Atrial Fibrillation in Daily Life
- Understand your condition: Learn about what atrial fibrillation is and how it affects your heart. Clear knowledge can improve treatment adherence.
- Healthy lifestyle habits: Lifestyle changes like regular exercise, a balanced diet, avoiding tobacco, reducing alcohol, and managing stress can significantly impact heart health.
- Take medications as prescribed: Follow your doctor’s advice on blood thinners and rhythm-control or rate-control medicines.
- Regular check-ups matter: Frequent monitoring helps with early detection of changes and adjusting treatment plans.
- Know when to seek help: Seek medical attention if symptoms get worse — like increased palpitations, dizziness, or shortness of breath.
Finding the Best Cardiology Doctor
Choosing the best cardiology doctor for atrial fibrillation care is very important. Here are easy tips to find the right specialist:
- Credentials matter: Look for a cardiologist with experience in heart rhythm disorders — especially one who specialises in electrophysiology (a sub-speciality that deals with abnormal heart rhythms).
- Experience with latest treatments: Ensure the doctor stays updated with the latest guidelines and treatments in atrial fibrillation, including catheter ablation and new anticoagulation options.
- Communication is key: The best cardiology doctor should listen carefully, explain things clearly in simple language, and involve you in decisions about your treatment.
- Consult multiple opinions: If unsure, consider getting a second opinion — especially before major procedures like ablation.
Final Thoughts
The 2026 update for managing atrial fibrillation brings a more balanced, evidence-based, and personalised model of care. These changes help doctors treat not just the heart rhythm but the whole person — focusing on stroke prevention, rhythm control, managing other health conditions, and involving patients in every step.
If you or someone you know has atrial fibrillation, work closely with a trusted cardiologist or the best cardiology doctor you can find. Good heart care is a team effort — combining expert medical guidance, safe medicines, a healthy lifestyle, and regular follow-ups.