Atrial Fibrillation (AF) is one of the most common heart rhythm disorders worldwide, affecting millions each year.
For many patients, medication alone is not enough to control symptoms such as palpitations, fatigue, breathlessness,
or the risk of stroke. This is where catheter ablation becomes a major treatment option.
Today, two major technologies dominate the AF ablation space:
Radiofrequency (RF) Ablation—the long-standing heat-based therapy, and
Pulsed Field Ablation (PFA)—a new, non-thermal, tissue-selective technology revolutionizing electrophysiology.
“PFA vs. RF Ablation—Which is better for treating Atrial Fibrillation?”
What Is Atrial Fibrillation and Why Is Ablation Needed?
Atrial Fibrillation is a condition in which the upper chambers of the heart beat irregularly and rapidly.
This disrupts blood flow and significantly increases the risk of stroke, heart failure, and cardiac arrest in severe cases.
Catheter ablation aims to isolate abnormal electrical signals—usually originating from the pulmonary veins—that trigger AF.
The goal is to create precise, safe lesions that stop erratic electrical circuits and restore normal rhythm.
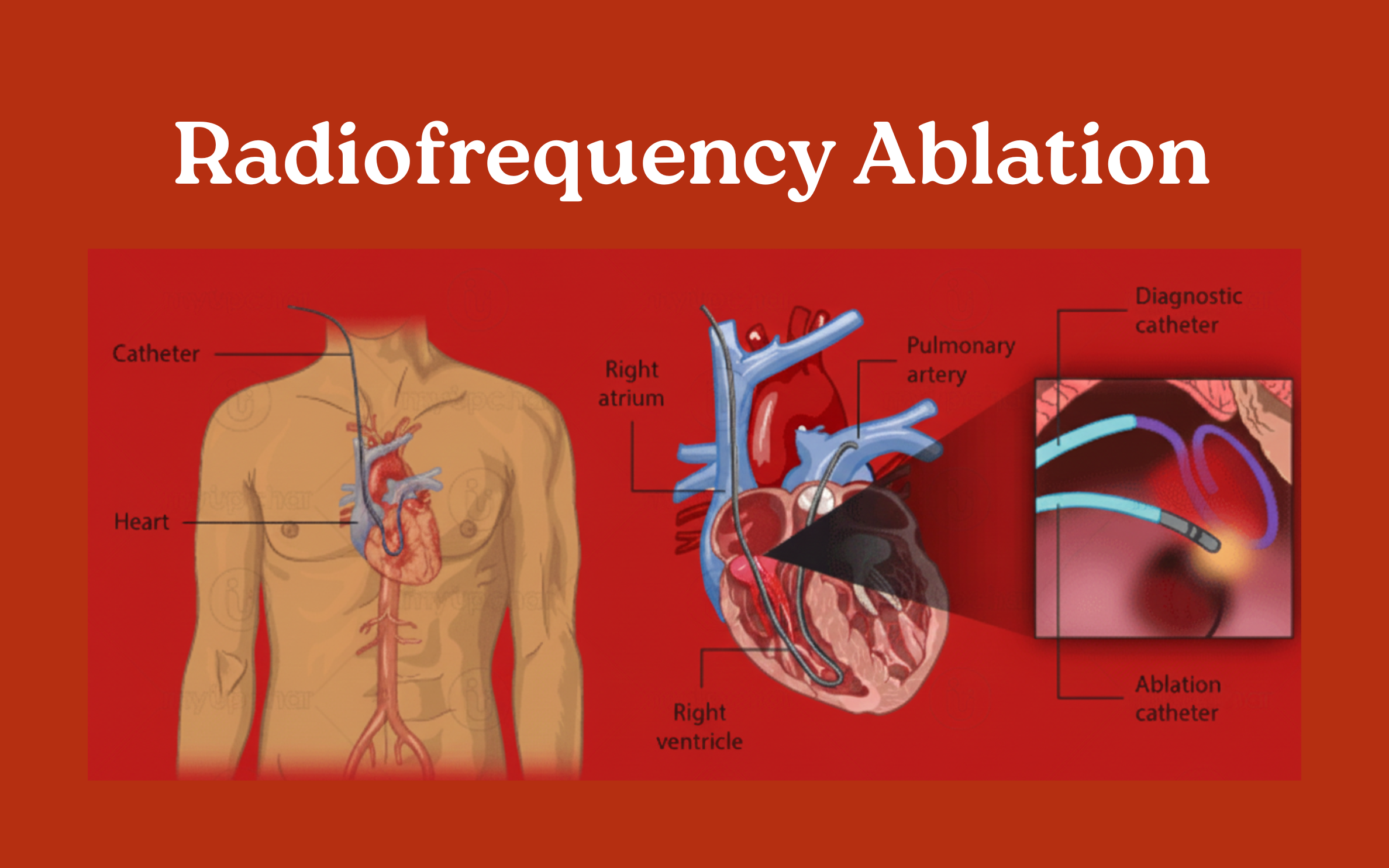
1. What Is RF Ablation? (Radiofrequency Ablation)
Radiofrequency Ablation has been the gold standard for more than two decades. It uses thermal energy (heat)
to destroy problematic heart tissue.
How RF Ablation Works
- A catheter is inserted into the heart through a blood vessel.
- High-frequency electrical energy is applied.
- Heat creates small lesions in the targeted tissue.
- These lesions block abnormal electrical pathways.
Advantages of RF Ablation
- Proven track record of safety and long-term success.
- Accurate and controlled lesion creation.
- Widely available in most heart centers.
- Effective for complex or persistent AF cases.
Limitations
- Heat can inadvertently affect nearby structures.
- Higher risk of complications such as esophageal injury, phrenic nerve damage, and pulmonary vein stenosis.
- Longer procedure and recovery times compared to PFA.
2. What Is PFA? (Pulsed Field Ablation)
Pulsed Field Ablation (PFA) uses non-thermal electrical fields rather than heat or cold.
It selectively targets cardiac cells while sparing surrounding tissues.
How PFA Works
- Ultra-short, high-voltage electrical pulses create microscopic pores in heart cells.
- This process, called irreversible electroporation, destroys only the intended tissue.
- Surrounding structures like the esophagus, nerves, and blood vessels remain largely unharmed.
Advantages of PFA
- Faster procedure time.
- Minimal collateral damage.
- Reduced complications.
- Safer for surrounding structures.
- Shorter recovery and hospital stay.
- High success rates, especially in first-time procedures.
Limitations
- Relatively new compared to RF ablation.
- Long-term (10+ years) outcome data is still evolving.
- Not yet available in all hospitals.
3. PFA vs. RF Ablation: Key Differences
| Feature | PFA (Pulsed Field Ablation) | RF Ablation (Radiofrequency) |
|---|---|---|
| Energy Source | Non-thermal electrical pulses | Thermal heat energy |
| Procedure Time | Faster | Longer |
| Safety | Very high; tissue-selective | Good but more collateral risk |
| Success Rate | High, especially in paroxysmal AF | High but more variable |
| Risk of Complications | Very low | Moderate |
| Risk of Cardiac Arrest | Extremely low | Low but possible |
| Recovery Time | Short | Longer |
| Availability | Rapidly expanding | Widely available |
4. Is PFA Safer Than RF Ablation?
One of the biggest advantages of PFA is its significantly improved safety profile. Because it does not rely on heat, the risk of thermal injury to nearby organs is minimal.
- Extremely low risk of esophageal injury.
- Significantly reduced phrenic nerve damage.
- Shorter procedure time and reduced anesthesia exposure.
5. Success Rates: Which One Performs Better?
PFA Success Rates:
- 80–90% success in paroxysmal AF.
- Low early recurrence rates in studies.
- Rapid and durable pulmonary vein isolation.
RF Ablation Success Rates:
- 70–85% success in paroxysmal AF.
- Highly effective for persistent AF.
- Strong long-term evidence base.
6. Risk of Cardiac Arrest During Ablation
While extremely rare, any invasive cardiac procedure carries a small risk.
RF ablation risks are typically related to heat-induced injury or inflammation.
PFA significantly lowers this theoretical risk by avoiding heat, minimizing deep tissue damage, and shortening procedure duration.
7. Patient Experience: Which Is Better?
With PFA:
- Procedure often under 60 minutes.
- Less pain or discomfort.
- Faster recovery and often same-day discharge.
With RF Ablation:
- Possible chest discomfort post-procedure.
- Longer hospital stay in some patients.
- Closer monitoring required.
8. Which Is Better—PFA or RF Ablation?
Choose PFA if you want:
- The latest and safest AF ablation technology.
- Minimal complication risk.
- Faster recovery and hospital discharge.
Choose RF Ablation if:
- You have complex or long-standing arrhythmias.
- You prefer a well-established therapy with decades of data.
- PFA is not available at your treatment center.
9. The Future of AF Treatment
Pulsed Field Ablation represents a major leap forward in electrophysiology.
With its precision, safety, speed, and tissue selectivity, experts believe PFA may soon become the first-line treatment for most AF patients.
Final Thoughts
Atrial Fibrillation is a serious condition that increases the risk of stroke, heart failure, and cardiac arrest if left untreated. While RF ablation remains a reliable and proven therapy, PFA is clearly redefining the future of AF management.
Patients should discuss both technologies with a qualified cardiac electrophysiologist to determine the most appropriate treatment optin.